What is a brain tumour?
What is a brain tumour?
A brain tumour is a collection of abnormal cells that are located somewhere on, or in, the brain. Brain tumours can form when abnormal cells grow and multiply out of control, resulting in a benign or malignant mass inside the skull.
Benign tumours grow slowly over time and are unlikely to spread to other parts of the body. This is in contrast to malignant tumours, also known as cancer, which is fast-growing and can spread to other parts of the brain and the spine.
There are two ways that children can develop a brain tumour. Most commonly, brain tumours in children arise from within their brains. However, tumours can also be ‘seeded’ from another tumour in a different organ in the child’s body. This is called a secondary brain tumour.
How many children does it affect?
Childhood brain cancers are rare. Between 2011 and 2015, 192 children in Australia were diagnosed each year with either a malignant or benign brain tumour. During this period, this equated to approximately 44 cases per million people, representing 25% of all childhood cancer cases diagnosed during this time.
What are the symptoms?
A number of symptoms can be present in a child with a brain tumour.
The symptoms a child experiences will likely vary depending on the location and size of the brain tumour. Some of the main symptoms in children include, but are not limited to:
- Headaches
- Nausea and vomiting
- Irritability
- Seizures
- Feeling lethargic
- Trouble balancing
- Loss of vision
- Facial droop
A child with a brain tumour may experience one or more of these symptoms at any given time.
How is a brain tumour diagnosed?
A brain tumour can be diagnosed in several ways.
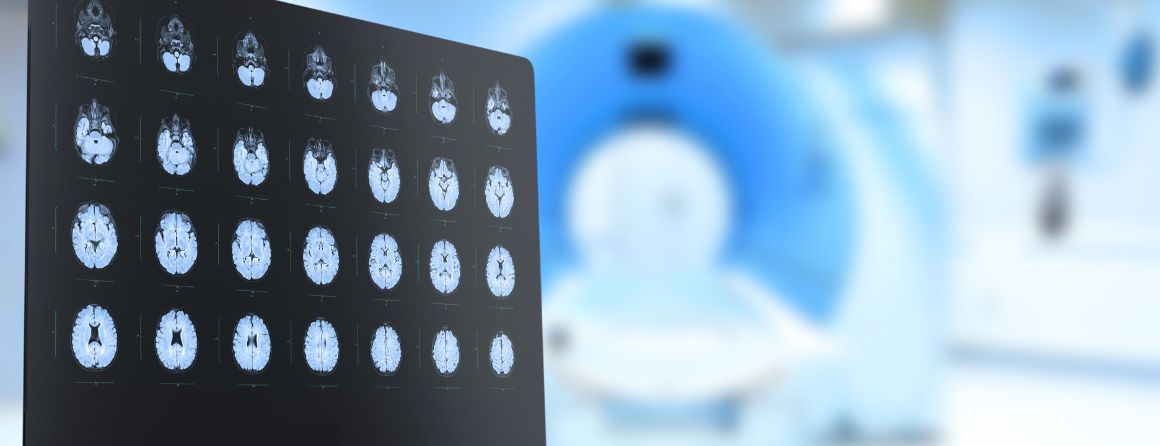
The most common way to diagnose a brain tumour is through magnetic resonance imaging (MRI). An MRI is a scan that gives a radiologist a detailed picture of a specific area of the body, such as the brain. This scan can confirm the presence of a brain tumour.
Often, a biopsy will need to be performed to characterise the exact type of tumour found on the brain. A biopsy is when a piece of the tumour is removed during surgery, allowing specialists to analyse it under a microscope or through molecular testing.
Specialists can also confirm the diagnosis of a brain tumour by analysing the fluid surrounding the brain and spine and/or specific blood markers.
How is it caused?
For most children who develop a brain tumour, the cause will remain unknown.
For other children, there may be a known genetic syndrome that increases their risk of developing a brain tumour. The most common is neurofibromatosis type 1 syndrome which can increase the risk of developing a type of tumour called a glioma, due to a mutation in the NF1 gene. Less frequently, a child may have Li-Fraumeni syndrome which has a mutation in the TP53 gene – a major gene responsible for preventing cells from becoming malignant.
There is only one recognised environmental factor that can increase the risk of a brain tumour. Radiation therapy, which is used to treat other types of cancer, can increase the risk of a tumour by exposing the head to significant radiation. There is no link between developing a brain tumour and mobile phone or electromagnetic field exposure.
What brain tumour research is taking place at Murdoch Children's Research Institute?
Murdoch Children’s Research Institute is working alongside the Children’s Cancer Centre (CCC) at The Royal Children’s Hospital and the Children’s Cancer Centre Biobank to better understand brain tumours in children and adolescence.
We are also a key partner in the Victorian Paediatric Cancer Consortium with the Hudson Institute and the Victorian Comprehensive Cancer Alliance.
These leading entities are highly regarded both nationally and internationally for their work, which is dedicated to giving all children the opportunity to live a healthy and fulfilled life.
Professor David Eisenstat and the Neuro-Oncology group at the Institute are studying brain differentiation programs to understand cancer development, in addition to promoting clinical and translational research on brain tumours and other paediatric cancers.
References:
Danny R Youlden, Peter D Baade, Adèle C Green, Patricia C Valery, Andrew S Moore and Joanne F Aitken Med J Aust 2020; 212 (3): 113-120. || doi: 10.5694/mja2.50456



