Researchers identify new rare genetic syndrome in children

Murdoch Children’s Research Institute researchers have identified a new rare genetic syndrome that causes intellectual disability and differences of sex development (DSD) in children.
The discovery paves the way for diagnoses in more affected individuals, providing families searching for answers with some certainty around this extremely rare disease. It could also lead to the development of new treatments.
Dr Katie Ayers and Professor Andrew Sinclair led the study, published in Nature Communications, which describes nine children from six families in Europe, Israel and North Africa who have intellectual disability, delays in reaching developmental milestone and neurodevelopmental (brain development) changes.
The children with male sex chromosomes (XY) also had a difference of sex development (atypical development or appearance of the gonads and external genitals). In these children, disruption to testis development (termed gonadal dysgenesis) meant reduced production of the masculinising hormone, testosterone, and female or atypical male genital appearance.
The team found that all affected children in these six families carry recessive variants in a gene called SART3, inherited from both parents. This is the first report of variants in the SART3 gene causing a congenital syndrome.
The researchers have suggested this new SART3-related condition be coined INDYGON (Intellectual Disability, Neurodevelopmental Defects and Developmental delay with 46,XY GONadal dysgenesis).
“The diagnosis of causative variants in the SART3 gene and INDYGON syndrome means the affected individual can be provided with the optimal clinical care and can access early support for their intellectual disability and developmental delay,” Dr. Ayers said. “Having a correct genetic diagnosis means that carrier testing is also possible for families.”
Dr Ayers said in many cases having a correct genetic diagnosis would also help the young person and their family to understand differences in their gonadal and genital development and inform decisions about potential therapeutic interventions.
Although it appeared that the children with SART3 variants and XX chromosomes had functional ovaries, some of these children are still young. Dr Ayers said, “Monitoring their developing ovaries is particularly crucial during and after puberty as if it is found that they are not functioning properly, hormone replacement may be necessary for their health and wellbeing. Similarly, children with XY chromosomes who did not develop fully functional testis may be at risk of developing gonadal cancer, which also requires monitoring.”
After finding the SART3 genetic changes, the team studied the molecular function of SART3 using fruit fly models and showed that the gene has a crucial role in testicular and brain development. They then introduced SART3 gene variants into human pluripotent stem cells and found that these cells had abnormal development in brain or gonadal models, which confirmed that the changes found in the affected children were the likely cause of disruptions to gonadal and neuronal development.
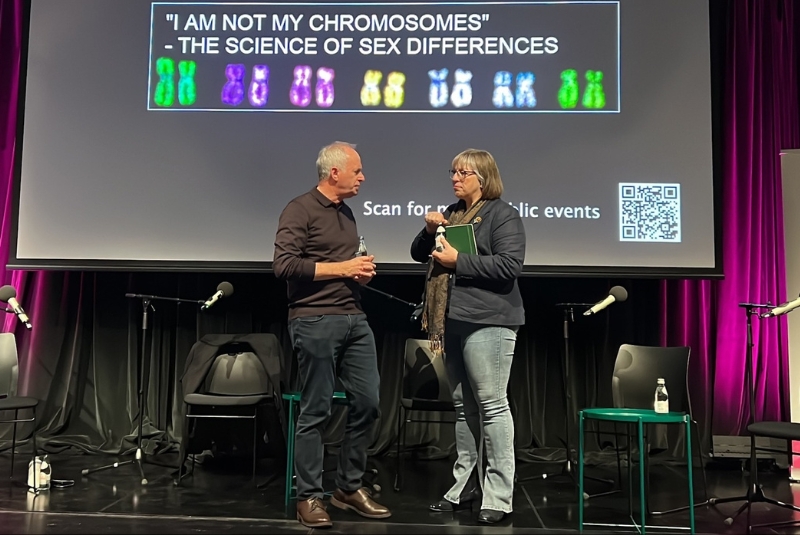
Professor Andrew Sinclair speaks about Differences of Sex Development on ABC's Big Ideas
As researchers now aim to better understand this new syndrome, and hope that in the future it may provide insight into how this condition arises and highlight new paths to treatments for these children.
This project has been conducted in collaboration with a number of parties as part of the grants supporting the study.
*The content of this communication is the sole responsibility of the Murdoch Children’s and does not reflect the views of the NHMRC.
Publication:
Katie L. Ayers, Stefanie Eggers, Ben N. Rollo, Katherine R. Smith, Nadia M. Davidson, Nicole A. Siddall, Liang Zhao, Josephine Bowles, Karin Weiss, Ginevra Zanni, Lydie Burglen, Shay Ben-Shachar, Jenny Rosensaft, Annick Raas-Rothschild, Anne Jørgensen, Ralf B. Schittenhelm, Cheng Huang, Gorjana Robevska, Jocelyn van den Bergen, Franca Casagranda, Justyna Cyza, Svenja Pachernegg, David K. Wright, Melanie Bahlo, Alicia Oshlack, Terrence J. O’Brien, Patrick Kwan, Peter Koopman, Gary R. Hime, Nadine Girard, Chen Hoffmann, Yuval Shilon, Amnon Zung, Enrico Bertini, Mathieu Milh, Bochra Ben Rhouma, Neila Belguith, Anu Bashamboo, Kenneth McElreavey, Ehud Banne, Naomi Weintrob, Bruria BenZeev and Andrew H. Sinclair. ‘Variants in SART3 cause a spliceosomopathy characterised by failure of testis development and neuronal defects,’ Nature Communications, DOI: 10.1038/s41467-023-39040-0
Funding
This research was supported by NHMRC Program Grant 546517 (2010-2014); NHMRC Program Grant 1074258 (2015-2019); NHMRC Ideas Grant (GNT1156942. 2018-2021).
Available for interview
Dr Katie Ayers, Murdoch Children’s Reproductive Development Co Group Leader
Media contact for Murdoch Children's
Phone: +61 457 365 848
Email:
show email address
About Murdoch Children's Research Institute
The Murdoch Children's Research Institute is the largest child health research institute in Australia committed to making discoveries and developing treatments to improve child and adolescent health in Australia and around the world. They are pioneering new treatments, trialling better vaccines and improving ways of diagnosing and helping sick babies, children and adolescents. It is one of the only research institutes in Australia to offer genetic testing to find answers for families of children with previously undiagnosed conditions.



