Immune cell model paves way for new treatments targeting common infection amongst immunocompromised children

Melbourne researchers have successfully engineered human immune cells to model an infection common among immunocompromised children in a breakthrough discovery, paving the way for new drug testing and treatments.
The research, led by the Murdoch Children’s Research Institute (MCRI) and published in Stem Cell Reports, used cutting-edge stem cell technology to better understand how the infection invades immune cells and causes health complications, such as lung and skin and soft tissue infections, in immunocompromised people, particularly those with cystic fibrosis.
Murdoch Children’s researcher Dr Shicheng Jacky Sun said the immune cell type the team created in the lab, known as a macrophage, played an important role in infection, inflammation and regeneration. But due to this function was also a natural host for germs.
“Using our stem cell-made immune cells, we successfully infected them with a germ called mycobacteria. We could see where these mycobacteria live inside human immune cells and the immune reactions they triggered,” he said.
“We were also able to use our stem cell model to rapidly test and screen different types of antibiotics against mycobacterium.”
Murdoch Children’s researcher Dr Sohinee Sarkar said the search for effective treatments had been hampered until now by the lack of infection models to test new drugs.
“Mycobacteria opportunistically infect people with lung diseases, such as cystic fibrosis, and also causes skin and soft tissue infections in those with immunodeficiencies,” she said.
“Current treatments take months and involve giving cocktails of different antibiotics with wide-ranging toxicities. Treatments often fail as the infection is highly resistant to antibiotics, leaving infected people with few other options. Patients with mycobacteria are also excluded from receiving life-saving lung transplants.
Dr Sarkar said due to high treatment failure rates, repeated cycles of infection could greatly damage the lung tissue and accelerate the progression of lung failure in those with cystic fibrosis.
“Improved treatments could mean less frequent hospital visits, shorter stays and minimal exposure to toxic antibiotics, which is particularly important for children with cystic fibrosis,” she said.
Data shows 11 per cent of children with cystic fibrosis test positive for mycobacteria.
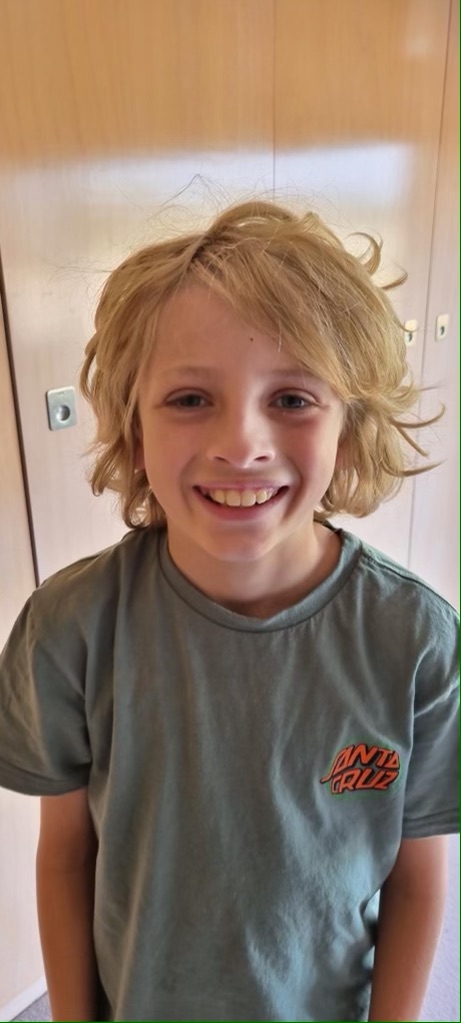 Rachell Regan’s son Wade, 11, who has cystic fibrosis, developed an infection caused by mycobacteria a year ago.
Rachell Regan’s son Wade, 11, who has cystic fibrosis, developed an infection caused by mycobacteria a year ago.
Rachell said despite trying several antibiotic treatments, none had managed to knock out the infection.
“His infection is very antibiotic resistant and none of the treatments have improved his condition,” she said. We just tried eight weeks of three different antibiotics, which all failed, and now he is trialling four types either taken intravenously, in tablet form or inhaled.
“Since Wade caught this infection, his lung function has dropped to 63 per cent, and that will continue to worsen if we can’t get on top of it. It’s hard when you are doing everything you can, and nothing seems to work.”
On top of the antibiotic treatment, which includes wearing a bag around his waist to help infuse the medication into his body, Wade has twice daily physio sessions and a nurse visits him every day at school.
 Rachell said the recent Murdoch Children’s research gave her hope that a successful treatment would be found.
Rachell said the recent Murdoch Children’s research gave her hope that a successful treatment would be found.
“The stem cell results are very reassuring that one day the right treatment will be discovered, which will be life-changing for Wade and other children who not only have a severe lung condition but have to grapple with infections too,” she said.
Dr Sarkar said the infection model could also be used for drug screening for other superbugs with limited treatment options.
“Some bacteria have evolved to escape our immune system by hiding themselves within host cells, making it difficult to treat these infections with traditional antibiotics,” she said. Our stem cell-based infection model can be readily scaled up to screen large number of drugs against such bacteria to identify new treatments.”
MCRI's Professor Ed Stanley, also a member of the new global stem cell medicine consortium, reNEW, added that the team was looking to extend and advance its stem cell research capability thanks to a $1 million business case from the State Government to see where Melbourne could best contribute to the global efforts to find treatments and therapies for a range of currently incurable conditions.
Researchers from the University of Melbourne and Monash University also contributed to the findings.
Publication: Shicheng Sun, Michael See, Hieu T. Nim, Kathleen Strumila, Elizabeth Ng, Alejandro Hidalgo, Mirana Ramialison, Philip Sutton, Andrew G. Elefanty, Sohinee Sarkar and Edouard G. Stanley. ‘Human pluripotent stem cell-derived macrophages host Mycobacterium abscessus infection,’ Stem Cell Reports. DOI: 10.1016/j.stemcr.2022.07.013
*The content of this communication is the sole responsibility of MCRI and does not reflect the views of the NHMRC.
Available for interview:
Dr Shicheng Jacky Sun, Murdoch Children’s researcher
Dr Sohinee Sarkar, Murdoch Children’s researcher
Professor Ed Stanley, Murdoch Children’s Theme Director, Stem Cell Medicine
Media Contact
Murdoch Children's Research Institute
Phone: show phone number
Email:
show email address
About the Murdoch Children’s Research Institute
The Murdoch Children's Research Institute is the largest child health research institute in Australia committed to making discoveries and developing treatments to improve child and adolescent health in Australia and around the world. They are pioneering new treatments, trialling better vaccines and improving ways of diagnosing and helping sick babies, children and adolescents. It is one of the only research institutes in Australia to offer genetic testing to find answers for families of children with previously undiagnosed conditions.
Funding:
This study was funded by the National Health & Medical Research Council of Australia through research fellowships awarded to A.G.E. (GNT1117596) and E.G.S (GNT1079004) and project grants awarded to A.G.E. and E.G.S. (GNT1129861, GNT1138717, GNT1123277), and by the Stafford Fox Medical Research Foundation. M.R. is funded by an NHMRC Ideas Grant (APP1180905). Additional infrastructure funding to the Murdoch Children’s Research Institute was provided by the Australian Government National Health and Medical Research Council Independent Research Institute Infrastructure Support Scheme and the Victorian Government’s Operational Infrastructure Support Program. The Australian Regenerative Medicine Institute is supported by grants from the State Government of Victoria and the Australian Government. The Novo Nordisk Foundation Center for Stem Cell Medicine is supported by Novo Nordisk Foundation grants (NNF21CC0073729).



